Why we can safely recycle food from hospital patient food trays
by Gary Kennedy *
Gary Kennedy
The Australian Government Department of Climate Change, Energy, the Environment and Water states on its website that food waste costs the Australian economy $36.6 billion each year – accounting for three per cent of Australia’s greenhouse gas emissions.
That website says Australia uses 2,600 gigalitres of water each year (equivalent to five Sydney Harbours) to grow food that is wasted – and the amount of land used to grow wasted food is larger than the state of Victoria.
FoodBank’s website estimates 18 per cent of all Australians are food insecure and says 36 per cent of all charities in Australia report they don’t have enough to feed all those who ask for food relief.
But the current procedures hospitals have in place say any food or drink brought to a patient or resident must be discarded on return to the kitchen and disposed of in the garbage/waste stream. This applies even to sealed, unopened items such as a can of lemonade, salt or sugar sachet, Vegemite PC pack or capped bottle of water.
The reason given for disposing of all food is “infection control”. This reason needs to be challenged.
Current legal status
When looking at the risk posed by re-using or donating food previously served to hospital patients, the relevant standards to consider within Australian food safety requirements are those within FSANZ’s Food Standard Code.
FSANZ Standard 3.1.1 [Interpretation and Application](5) says food must be “safe and suitable.”
The FSANZ Food Standards Code 3.2.2 [Food Safety Practices and General Requirements] (6) says under section 11 Food Disposal:
• “(4) A food business must not sell food that has been already served to a person to another person unless the food was completely wrapped when served and has remained completely wrapped.”
FSANZ Standard 3.3.1 [Food Safety Program for Food Service to Vulnerable Persons](7) makes minimal mention of handling or processing conditions, apart from describing activities considered “processing.”
There is nothing in the Food Standards Code that bans the practice of food donation from hospital trays, or the re-use of items including food items between different patients.
The NSW Food Authority’s “Guidelines for Food Service to Vulnerable Persons” (12) states similar requirements and does not mention re-use of food items specifically as an issue.
The current NSW Infection control document “Clinical Excellence Commission “Infection Prevention and Control Practice Handbook” (4) allows items to remain in hospital rooms between patients, provided effective infection control procedures are in place and followed.
So provided risk assessment and effective control measures are in place, medical and non-medical items that have been present for one patient are allowed to be in the same room when the next patient arrives – under current infection control protocols.
There is no Federal, State or Territory document that specifically states food from hospital trays cannot be donated to charity or re-used. In fact the reverse is true – the practice IS allowed.
Microbial Infection Risk
Do microbes capable of causing food poisoning and disease last for long periods on dry surfaces at ambient conditions?
The answer is yes. Many pathogens survive long periods at ambient.
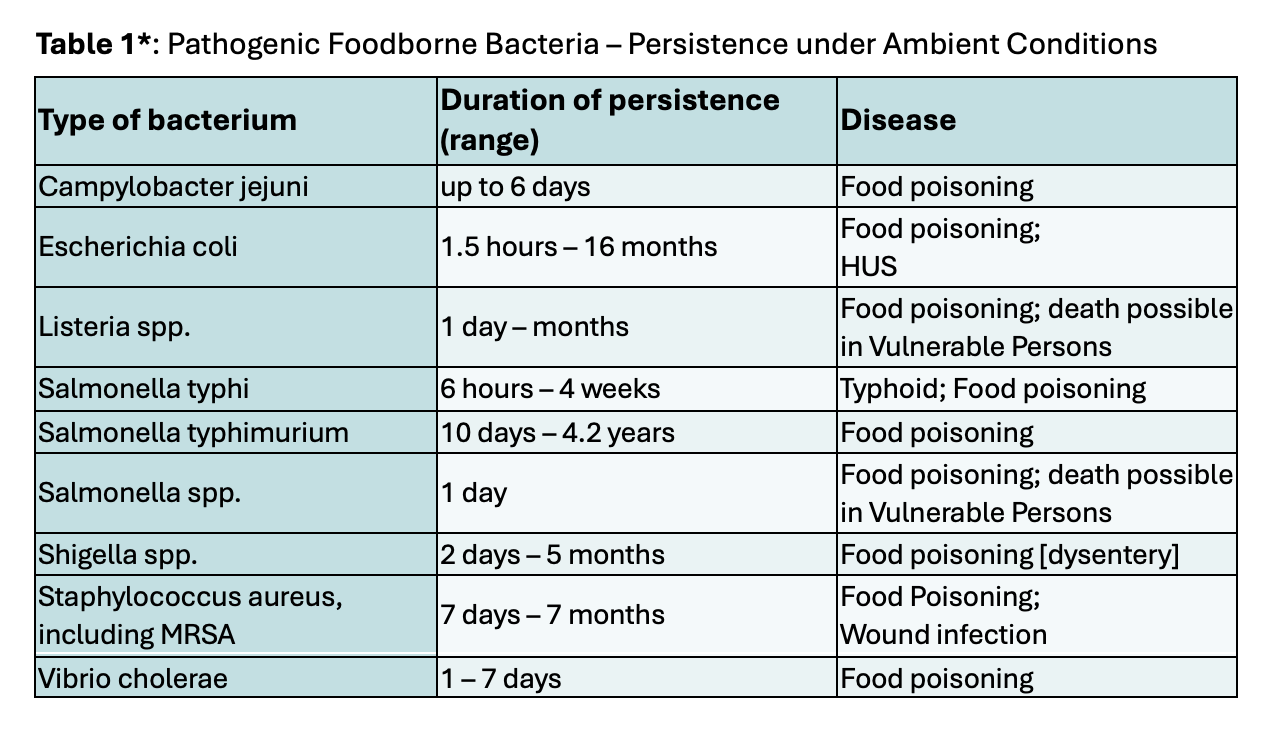
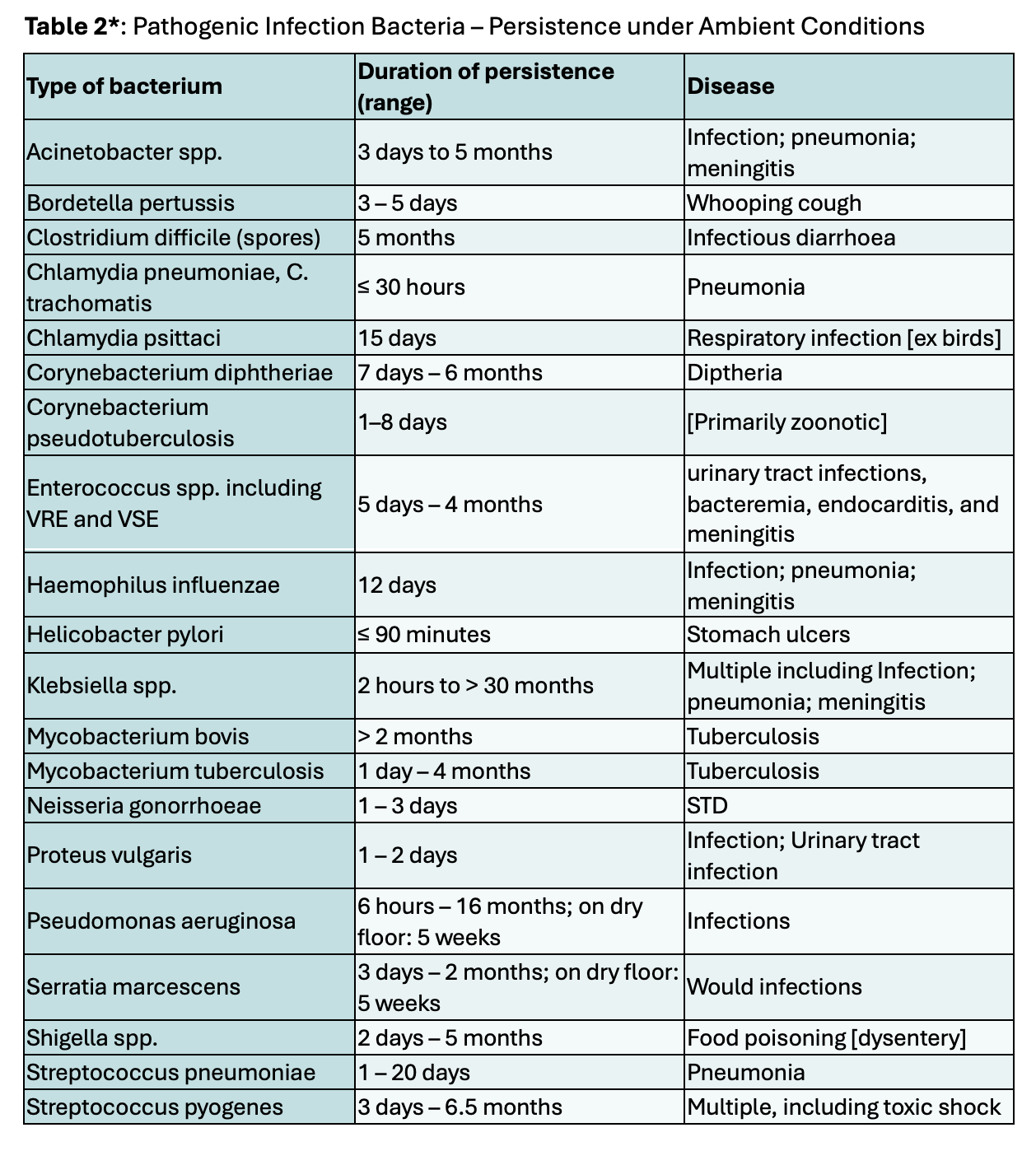
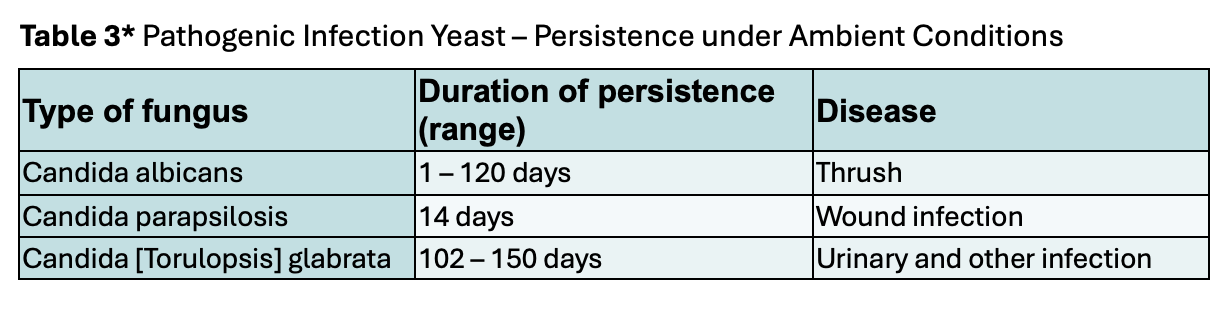
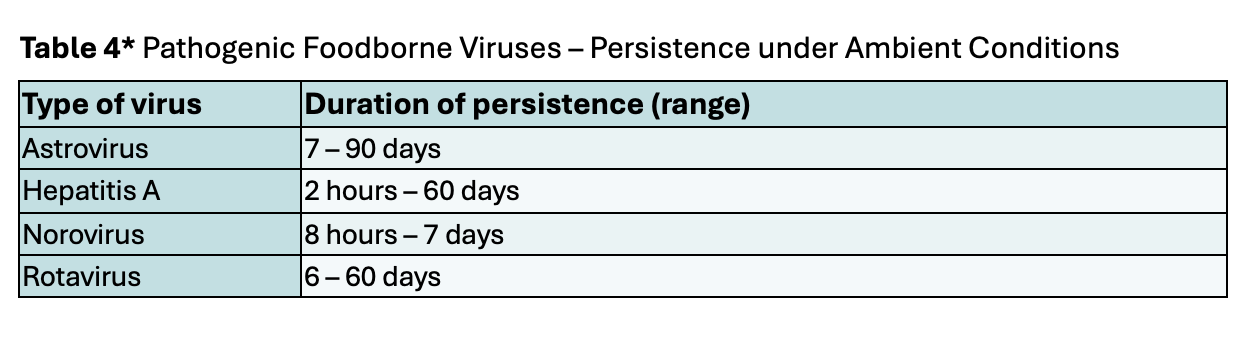
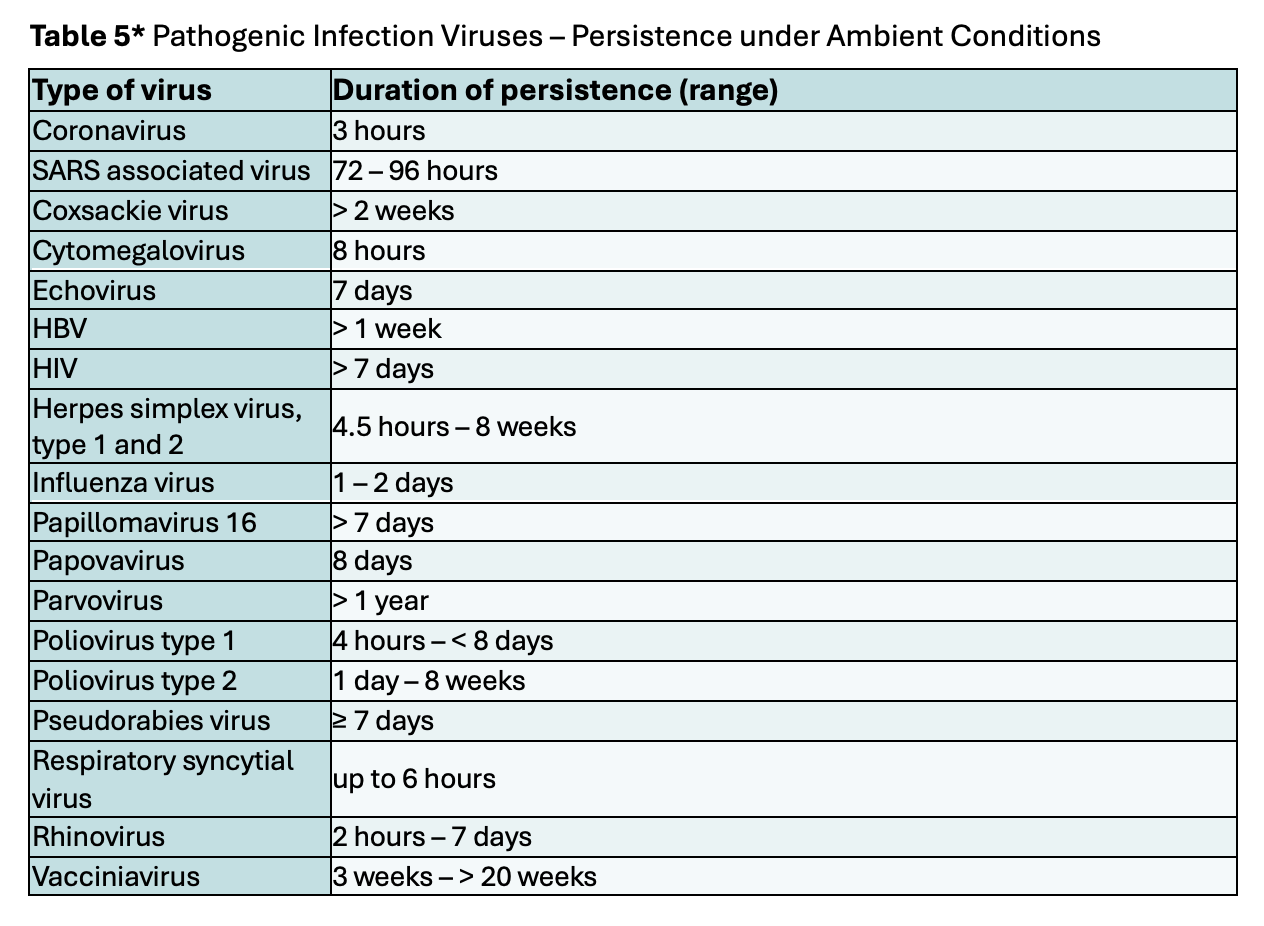
* Tables 1-5 derived from primarily from reference 9, updated for references 1, 2, 8, 10, 11, 13 & 14
An overall conclusion from these tables is that while many pathogens will die promptly when exposed to air, many will persist for long periods.
But, have there been recorded incidents of food poisoning or infection occurring from the exterior of food packaging?
No. There has never been a published case where an hospital acquired infection had been traced to pathogens on the outside of a food container. Nor has there been any published case where a case of food poisoning or infection has been traced to pathogens on the outside of a food container ever, anywhere in the world.
Published data originating from China in 2022 indicated COVID-19 outbreaks had originated from the COVID-19 being on the outside of frozen imported seafood(3). However, the FSANZ website states “The World Health Organization (WHO) advises that there is currently no evidence that people can catch COVID-19 from food or food packaging.”
Current Australian hospital operating practices
There is precedent for items being used between multiple patients within Australian public hospitals. Many non-consumable items stay in rooms between patients, such as boxes of gloves, vases and tissue boxes – all of which patients may access.
In Emergency wards, large amounts of sterile, clinical items are in easy reach of patients within the rooms and are not discarded between patients [following infection control guidelines].
Corridors in hospitals have trolleys of sterile consumables that can be touched by any patient or visitor passing by. These are not disposed of between patients as an infection control risk.
There is also precedent within foodservices. The majority of hospital wards have fridges and pantries where patients and visitors can access pre-packaged food after hours. This occurs commonly in maternity wards at larger hospitals, but at some sites may also occur in units such as renal and patient transport.
Pantries exist on many wards where patients can make themselves hot beverages and have a snack such as a biscuit. Ice machines in many hospital wards have patient and visitor access. A patient here may handle a product that has been previously touched by multiple hands of other patients, staff or visitors. No infection control issues are ever raised on these practices.
Items on trays bought up to hospital wards by foodservice departments are rarely washed or sanitised within foodservices, yet they may have originated in factories and in warehouses all over the world. Whatever was on the outside of the packet when the product was delivered to the hospital dock goes to the patient for them to touch by hand and, for some products, to raise up to and touch their lips. This is not raised by infection control as a risk.
In longstay hospitals in recent years, changes have been occurring to make dining rooms more like home, bringing back sugar bowls, jars of condiments on the table and the like. Currently items such as sauce bottles and portion control condiments sit on tables where any longstay patients, residents and visitors can touch them. All of this meets current applicable infection control guidelines.
Further, there is precedent for the re-use of items from the food tray already served to a patient. At many hospital sites in Australia, enteral feeds are delivered to wards on patient food trays by the foodservices staff. Those that are unused and returned on patient trays to the kitchen are taken off the trays and used for subsequent patients without sanitising.
Typical ambient shelf stable foods that could be suitable for donation to charity and are currently discarded include:
• Canned, bottled and UHT [longlife] drinks including water, soft drinks, flavoured milk, fruit juice and juice drinks, ready-to-drink cordials and formulated beverages [eg Sustagen]
• Fruit cups, shelf stable jellies, shelf stable ambient desserts [eg fruit cake slices]
• Packaged dry portioned controlled dry goods including biscuits, breakfast cereals, portion-controlled condiments, muesli bars, ambient cheese portions
• Coffee sachets and tea bags, sugar and sweetener sachets
• Longlife milk portions
Of course there would be some limitations. Opened packages would not meet the Food Standards Code if reused, and food from high risk infections rooms and wards should continue to be discarded and not re-used or donated.
With some risk assessment and controls put in place, there is no reason this system could not be expanded to include chilled and frozen food, and even hot food from hospital foodservice where “fully wrapped” as per the FSANZ Food Standard Code Standard 3.1.1. (5)
Chilled, frozen and hot food are already being donated to food relief charities in Australia without issue.
To conclude: while we get told all unopened food on a patient’s tray must be binned and wasted, there seems little reason to do this – if we can show the food is still safe and meets the food safety laws.
References:
1. Bean. B et al 2014. Survival of Influenza Virus on Environmental Surfaces. The Journal of Infectious Diseases. Vol 146.1 PP47-51
2. Centre for Disease Control 2008. Guideline for Disinfection and Sterilisation in Healthcare facilities. 158pp.
3. China CDC Weekly COVID-19 Outbreaks Linked to Imported Frozen Food in China: Status and Challenge. 2022 Jun 3; 4(22):483–487
4. Clinical Excellence Commission 28 August 2017. Infection Prevention and Control Practice Handbook
5. Food Standards Australia New Zealand [FSANZ], 19 July 2023. Standard 3.1.1, Interpretation and Application. From www.foodstandards.gov.au
6. Food Standards Australia New Zealand [FSANZ], 19 July 2023. Standard 3.2.2, Food Safety Practices and General Requirements. From www.foodstandards.gov.au
7. Food Standards Australia New Zealand [FSANZ], 11 July 2021. Standard 3.3.1. Food Safety Program for Food Service to Vulnerable Persons. From www.foodstandards.gov.au
8. HCV Advocate [org] 2015. Environmental Stability of HCV: How Long Does HCV Live Outside the Body and What Kills It? HCV Fact Sheet V5.2 From www.hcvadvocate.org
9. Kramer. A, Schwebke. I and Kamp. G. 2006. How long do nonsocmial pathogens persist on inanimate surfaces? A systematic review. BMC Infectious Diseases 2006 6:130
10.Mayo Clinic USA, 24 Feb 24. How long do cold and flu germs stay alive after infected people cough or sneeze? From www.mayoclinic.org
11.National Health Service UK 2015. How long do bacteria and viruses line outside the body? From www.nhs.uk
12.NSW Food Authority 2016. Guidelines for Food Service to Vulnerable Persons. From www.foodauthority.nsw.gov.au
13.Shamin. A et al. 1988. Rotavirus Survival on Human Hands and Transfer of Infectious Virus to Animate and Non-Porous Inanimate Surfaces. Journal of Clinical Microbiology, Aug 1988, p 1513 – 1518
14.Stowell. J et al. 2012. Cytomegalovirus Survival on Common Environmental Surfaces Opportunities for Viral Transmission. The Journal of Infectious Diseases. Volume 205, Issue 2, 2012 Pages 211–214
* Hospitality in Healthcare Life Member Gary Kennedy is a Food Auditor and Manager of Correct Food Systems